Psoriasis
Reduce plaque formation with Vitop Psoricur
What is psoriasis?
Plaque psoriasis (psoriasis vulgaris) is a chronic, relapsing skin disease. The underlying autoimmune condition causes the body to perceive its own skin cells as foreign, triggering inflammation in the skin. This is accompanied by disrupted skin cell formation, as the accelerated renewal process prevents their full maturation. The resulting cell clusters accumulate on the skin's surface, forming scaly plaques.
This most common form of psoriasis is also known as psoriasis vulgaris or plaque psoriasis. Other forms exist and are classified according to their location, appearance, or the age of the person affected. Examples include pustular psoriasis and guttate psoriasis.
What symptoms indicate psoriasis?
The most common symptom is the appearance of so-called “plaques”. These are silvery-white, scaly patches that typically develop on reddened, inflamed areas of the skin. Their size and severity can vary, and they are often accompanied by itching and/or a sensation of tension.
You would like to have a look at our product recommendations directly?
Plaque psoriasis is the most common form of the condition, affecting 80-90% of all people with psoriasis.
Symptoms: Plaques (silvery-white scales) on reddened areas of skin, often accompanied by itching or a burning sensation
Commonly affected areas of the body: Elbows, knees, torso, face, behind the ears, hands, and feet
Guttate psoriasis affects only a small number of people with psoriasis, mainly children and adolescents. This form of psoriasis usually occurs as a result of an infectious disease (e.g. a streptococcal infection). While it often resolves with the infection, psoriasis vulgaris may develop later in life in some cases.
Symptoms: “Guttata” is Latin for “drop-shaped,” referring to the numerous small, red psoriasis lesions that appear in a scattered, droplet-like pattern.
Commonly affected areas of the body: Torso, arms and legs
Inverse psoriasis typically affects skin folds. Since these areas of the skin are exposed to more moisture and friction, the typical flaking is often absent. Overweight individuals are at higher risk of inverse psoriasis.
Symptoms: Sharply defined red patches, often oozing and itching
Commonly affected areas of the body: Armpits, below the breasts, gluteal and genital folds
This rare form of psoriasis is accompanied by purulent blisters and, like inverse psoriasis, often lacks the typical scaling.
Symptoms: White, pus-filled, non-infectious blisters that turn into brownish crusts. May be accompanied by fever in rare cases.
Commonly affected areas of the body: Distributed over a wide area of the body (generalised pustular psoriasis) or limited to a specific region, such as the palms (palmar pustular psoriasis)
Scalp plaques are a common psoriasis symptom. In medical terms, this is referred to as “psoriasis capitis”.
Symptoms: Reddened and heavily scaly skin lesions (plaques) that usually itch. In some cases, psoriasis capitis can also lead to hair loss.
Commonly affected areas of the body: Hairy and hairless parts of the scalp, hairline.
Around 50% of people with psoriasis also experience symptoms on their fingernails and/or toenails.
Symptoms: Pitted nails (dimples in the nails), "oil spots" (brownish discolouration), grooves, and nail detachment
Commonly affected areas of the body: Toenails, fingernails
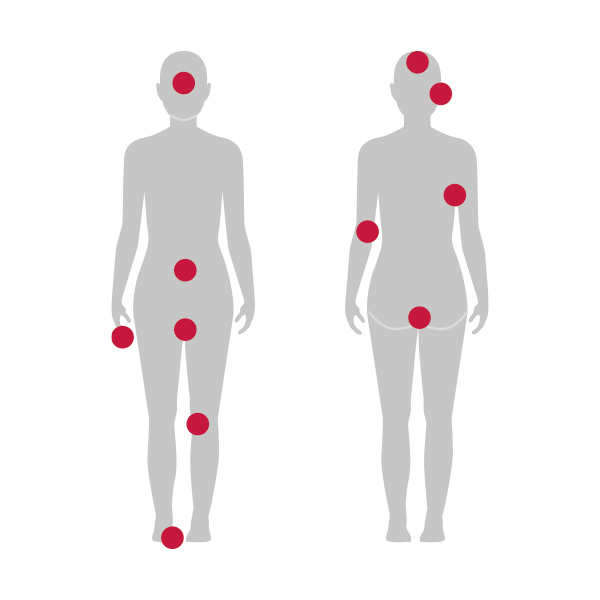
Commonly affected areas of the body in psoriasis
Plaque psoriasis typically appears in one or more of the following areas of the body:
- Extensor surfaces of joints and extremities (elbows, knees)
- Face
- Scalp and behind the ears
- Toenails and fingernails
- Armpits
- Lower back/gluteal fold
- Belly button
- Intimate area
Psoriasis is not contagious
Whether someone develops psoriasis is mainly determined by genetic factors. Transmission, such as through contact, is not possible
There are two types of psoriasis
Type I (early onset): Onset before the age of 40, usually with a more severe course
Type II (late onset): Onset after the age of 40, usually with a milder course
Around 125 million people affected worldwide
Like atopic dermatitis, psoriasis is among the most common skin conditions globally. According to estimates by the World Health Organization (WHO), it affects roughly 2–3% of the global population.
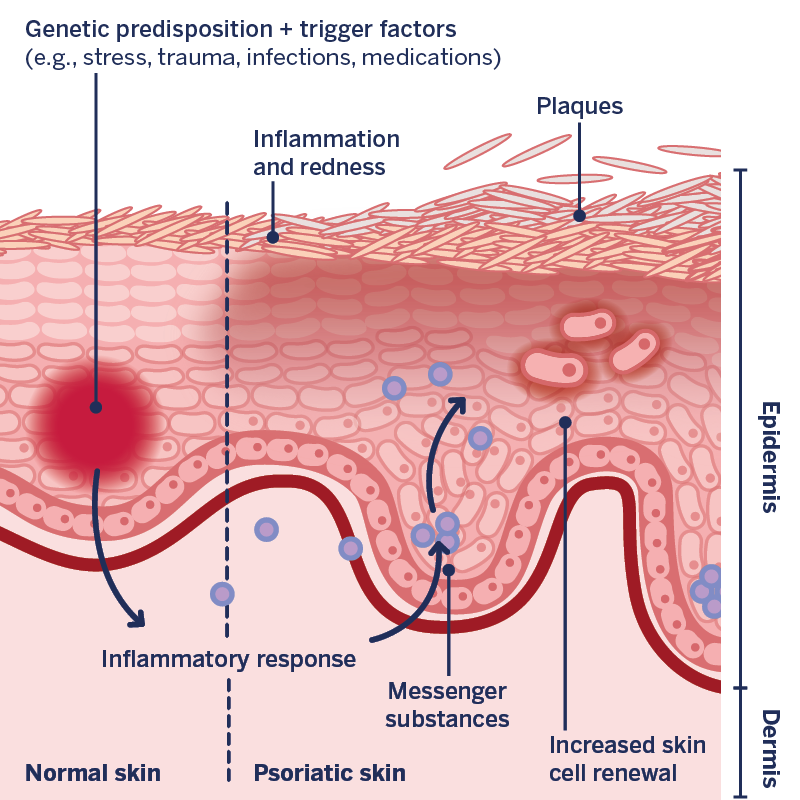
Causes and development of psoriasis
Genetic predisposition: Although the exact mechanisms have not yet been identified, genes are known to play an important role in psoriasis. As a result, children of parents with psoriasis have a higher risk of developing the condition themselves.
Trigger factors: Genetic predisposition alone does not cause the disease. An outbreak or flare-up typically occurs only when individual factors trigger the condition. These may include stress, certain medications, or infections.
Immune system: When a genetic predisposition combines with individual trigger factors, the typical symptoms of psoriasis may develop. These result from a misdirected response of the immune system, in which the body confuses its natural skin cells with harmful proteins. The immune system then releases messenger substances that prompt the body to attack its own cells, triggering inflammation. This inflammation leads to redness, itching, and an excessive renewal of skin cells, resulting in the formation of the characteristic scaly patches or plaques.

DERMASENCE has developed a powerful product duo as a systemic care product for psoriasis (scaly and inflammation-prone skin with heavy plaque formation).
DERMASENCE Vitop Psoricur Acute care cream with the innovative anti-proliferative woad extract (AP)
- Helps in prolonging periods without flare-ups in psoriatic skin conditions1
- Reduces excessive accumulation of scales and plaques
- Soothes irritated skin and prevents inflammation
DERMASENCE Adtop 40% Urea Oleogel
- Intensive care for flaking and severely keratinised skin
- Provides a keratolytic (scale-softening) and skin-smoothing effect
Real effectiveness – scientifically proven
DERMASENCE has demonstrated the effectiveness of Vitop Psoricur Acute care cream in a clinical study involving 16 participants with dry, psoriasis-prone skin.
1 Confirmed in a study
Participants applied DERMASENCE Vitop Psoricur acute care cream during four weeks. The result:
- 100% confirmed that the product regenerates and strengthens the skin.
- 93% reported that the product helps in prolonging periods without flare-ups in psoriatic skin conditions.
- 93% observed a visible reduction in skin redness.
- 93% confirmed a noticeable reduction in scaling.
Sources
- Mrowietz U.; Prinz J. C. (2018): Psoriasis. In: Plewig, G./Ruzicka, T./ Kaufmann, R./Hertl, M. (eds.). Braun-Falco’s Dermatologie, Venerologie und Allergologie. 7th edition. Berlin, Springer Reference Medizin. p 677-702.
- Boehncke W.H.; Schön M.P. (2015): Psoriasis. In: Lancet. Issue 386. p 983-94. doi: 10.1016/S0140-6736(14)61909-7.
- German Dermatological Society; Professional Association of German Dermatologists (2021): S3 guideline for the treatment of plaque psoriasis – adapted from EuroGuiDerm. AWMF registration number 013-001. In: AWMF online.
- Armstrong A.W.; Read C. (2020): Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: A Review. In: JAMA. Issue 323. p 1945-1960. doi: 10.1001/jama.2020.4006. PMID: 32427307.
- Rendon A.; Schäkel K. (2019): Psoriasis Pathogenesis and Treatment. In: Int J Mol Sci. Issue 6. doi: 10.3390/ijms20061475. PMID: 30909615; PMCID: PMC6471628.